
Skin conditions are among the most common health issues worldwide, impacting millions and posing significant challenges to healthcare systems. From the relentless itch of atopic dermatitis to the inflamed patches of psoriasis and the stark depigmentation caused by vitiligo, these conditions affect both physical health and mental well-being.
As the prevalence of chronic skin diseases continues to rise, so does the demand for effective, long-lasting treatments. Yet, despite ongoing dermatology clinical trials, many patients still struggle to find therapies that offer lasting relief and complete disease management remains an ongoing challenge. This reality highlights an urgent unmet medical need.
Dermatology Clinical Research Organisations like Comac Medical play a vital role in advancing the field, supporting the development and execution of well-designed trials that pave the way for more targeted and effective treatments.
In this article we will explore into the factors driving the demand of dermatology clinical trials, discuss the critical role of clinical research organisations and highlight now Comac Medical is contributing to progress in the field and illustrate with a successful case study on Atopic Dermatitis.
The Growing Demand for Dermatology Clinical Trials
Rising Prevalence of Chronic Skin Diseases Worldwide
Unfortunately, many chronic skin conditions like atopic dermatitis, psoriasis, and vitiligo have been associated with steadily rising prevalence, which may be driven by factors such as genetics, environmental influences, and lifestyle changes. Moreover, these conditions not only manifest physically but also significantly affect patients’ psychological and social well-being. Naturally, problems require solution, and thus, this increasing demand for solutions is creating an urgent need for innovative and effective treatments.
Among the most prevalent skin conditions are atopic dermatitis, psoriasis and vitiligo, let us recap and explore the nature and definition of these diseases in further detail below:
Atopic Dermatitis (AD): A chronic inflammatory skin disease characterised by red, itchy, and inflamed patches, often appearing in early childhood but persisting into adulthood. Affecting around 15-20% of children and 1-3% of adults globally, AD can significantly impair quality of life, causing sleep disturbances, social isolation, and psychological distress.
Psoriasis: An autoimmune disorder that results in red, scaly, and often painful patches on the skin, commonly found on the elbows, knees, and scalp. Affecting approximately 2-3% of the global population, psoriasis is linked to other comorbidities, including cardiovascular disease and mental health challenges.
Vitiligo: A chronic condition where the skin loses its pigment or “colour”, forming white patches that can appear anywhere on the body. Caused by the destruction of melanocytes, vitiligo affects 0.5-2% of people worldwide and is often accompanied by stigma and reduced self-esteem.
Growing Awareness of the Impacts of Dermatological Conditions
In addition, to the rising prevalence, there is also a growing awareness of psychological and social impacts of the skin conditions, alongside the painful physical symptoms, chronic skin conditions take a major toll on mental health and social interactions. Patients with atopic dermatitis often endure chronic itching and visible flare-ups, leading to sleep disturbances, anxiety, and depression. Psoriasis can cause pain and deep-seated discomfort, while also exposing patients to stigma and social isolation. Vitiligo, particularly when visible on the face or hands, can result in reduced self-esteem and possible discrimination.
As a result, both patients and healthcare providers are advocating for more comprehensive and robust treatments. Dermatology clinical research plays a pivotal role in addressing these needs by exploring therapies that not only alleviate symptoms but also improve the overall quality of life for patients.
The Increasing Need for Personalised and Targeted Treatments
Chronic skin conditions are often unpredictable and vary significantly between individuals. Atopic dermatitis, for example, may manifest differently based on age and ethnicity, while psoriasis severity can range from mild plaques to widespread inflammation. Vitiligo presents unique challenges due to its variable patterns of pigmentation loss.
Personalised and targeted treatments are essential in achieving optimal outcomes, as one-size-fits-all therapies often fail to address individual patient needs. Dermatology clinical studies help identify biomarkers and genetic factors that influence disease progression and treatment response, enabling the development of more tailored therapies.
Why Dermatology Clinical Trials Are Essential
Clinical trials provide the foundation for developing novel therapies and optimising existing ones. From topical treatments to systemic biologics, every advancement in dermatology emerges through rigorous clinical research.
Moreover, skin conditions like psoriasis and vitiligo often originate from complex immune dysregulation and genetic predispositions. Clinical trials allow researchers to study these mechanisms in diverse patient populations, leading to more accurate diagnostics and improved therapeutic approaches.
In addition, for many patients’, dermatology clinical trials allow the participation in a clinical trial, which is an opportunity to receive advanced care that may not be available through standard treatment options. Trials focusing on severe or treatment-resistant cases offer hope to those who have exhausted conventional therapies.

Addressing Challenges in Dermatology Clinical Trials
Conducting dermatology clinical studies presents unique challenges that can significantly impact the success and reliability of study outcomes. Due to the chronic and often fluctuating nature of skin conditions like atopic dermatitis, psoriasis, and vitiligo, recruiting and retaining patients for clinical trials can be particularly difficult.
Patient Recruitment and Retention
One of the primary challenges in dermatology clinical trial recruiting is patient retention, as the chronic nature of these diseases may discourage long-term commitment. Many trials require frequent hospital visits, prolonged treatment regimens, and strict monitoring, often involving repeated testing and skin assessments. These demands can become burdensome for participants, leading to high dropout rates and protocol deviations.
Additionally, many patients with chronic skin conditions experience periods of improvement and relapse, which can make them hesitant to commit to lengthy trials. Ensuring patient adherence to trial protocols and follow-up visits requires maintaining high levels of motivation and engagement throughout the study, especially when unforeseen challenges arise. Incorporating adaptive trial designs and rescue study strategies can help address recruitment and retention issues. This is often best achieved in specialised dermatology clinical research centres, where experienced teams can provide dedicated patient support and effective communication strategies to keep participants motivated.
However, conducting clinical trials in Central and Eastern Europe (CEE) has proven advantageous in overcoming some of these challenges, thanks to the region’s high patient availability and robust healthcare infrastructure. These factors not only support efficient recruitment but also improve patient retention by minimising burdens related to accessibility and follow-up care.
Variability in Disease Presentation
Another key challenge in dermatology clinical research is the variability in disease presentation and symptom severity among patients. Skin conditions like psoriasis and atopic dermatitis can range from mild, localised patches to severe, widespread involvement. This variability complicates the standardisation of trial protocols and can lead to inconsistencies in data collection. In addition, certain conditions, such as vitiligo, may progress or stabilise unpredictably, making it challenging to assess treatment efficacy within a fixed trial period. To address this, dermatology CROs often develop comprehensive eligibility criteria and utilise validated scoring systems, like the Psoriasis Area and Severity Index (PASI) or the Eczema Area and Severity Index (EASI), to maintain consistency in assessing disease severity and treatment response.
Placebo Effects and Subjective Reporting
Placebo effects and subjective reporting of symptoms can also skew data accuracy in dermatology clinical trials. Since many dermatological conditions cause visible and physically uncomfortable symptoms, participants may perceive improvements based on psychological factors rather than the actual efficacy of the investigational product. Furthermore, the reporting symptoms like itching or pain can introduce bias. To mitigate this risk, dermatology clinical research organisations often incorporate objective measurement techniques, such as digital imaging analysis or biomarkers, to complement patient-reported outcomes. Implementing double-blind, placebo-controlled designs also helps minimise bias and enhance data integrity.
Seasonal Variability and Environmental Factors
Seasonal variations and environmental factors pose additional challenges in dermatology clinical studies, as they can influence disease severity. For example, psoriasis may worsen in colder, drier climates due to reduced humidity and increased skin dryness, while atopic dermatitis often flares up in winter when indoor heating causes skin dehydration. Conversely, conditions like vitiligo may become more apparent in summer when tanning accentuates depigmented areas. Additionally, environmental pollutants and allergens can exacerbate symptoms, making it difficult to attribute changes solely to the investigational product. To account for these factors, trials must carefully consider the timing and geographic location of the study and may implement strategies like stratified randomisation to balance seasonal impacts across treatment groups.
Heterogeneous Patient Populations
Heterogeneous patient populations introduce variability in treatment responses, which can complicate the interpretation of trial results. Genetic differences, comorbid conditions, and variations in lifestyle factors, such as diet and skincare routines, can all influence outcomes. Recruiting a diverse yet well-defined patient cohort is essential to producing generalisable and reliable data. Advanced data analytics and subgroup analysis can further help identify patterns and assess how demographic and genetic factors affect treatment efficacy.
The Role of CROs in Advancing Dermatology Clinical Research
Contract Research Organisations streamline study processes and ensuring high-quality data collection. By leveraging industry expertise and applying innovative solutions, CROs facilitate the successful execution of clinical trials, helping sponsors to navigate the complexities of dermatological research. CROs also contribute comprehensive patient recruitment strategies, and the use of advanced technology for data collection and monitoring are key components of their support. This holistic approach significantly enhances the efficiency and accuracy of dermatology clinical trials, ultimately leading to more reliable and impactful outcomes.
To address these challenges, dermatology CROs like Comac Medical implement patient-centric approaches to dermatology clinical trial recruiting, and utilises rigorous monitoring, and adaptive trial designs to ensure reliable and robust data collection for trial protocol optimisation.
Comac Medical’s Dermatology Experience
At Comac Medical, we take pride in our commitment to conducting successful dermatology clinical research. Our numereous specialised services combine cutting-edge trial design with a patient-cantered strategy to ensure optimal outcomes.
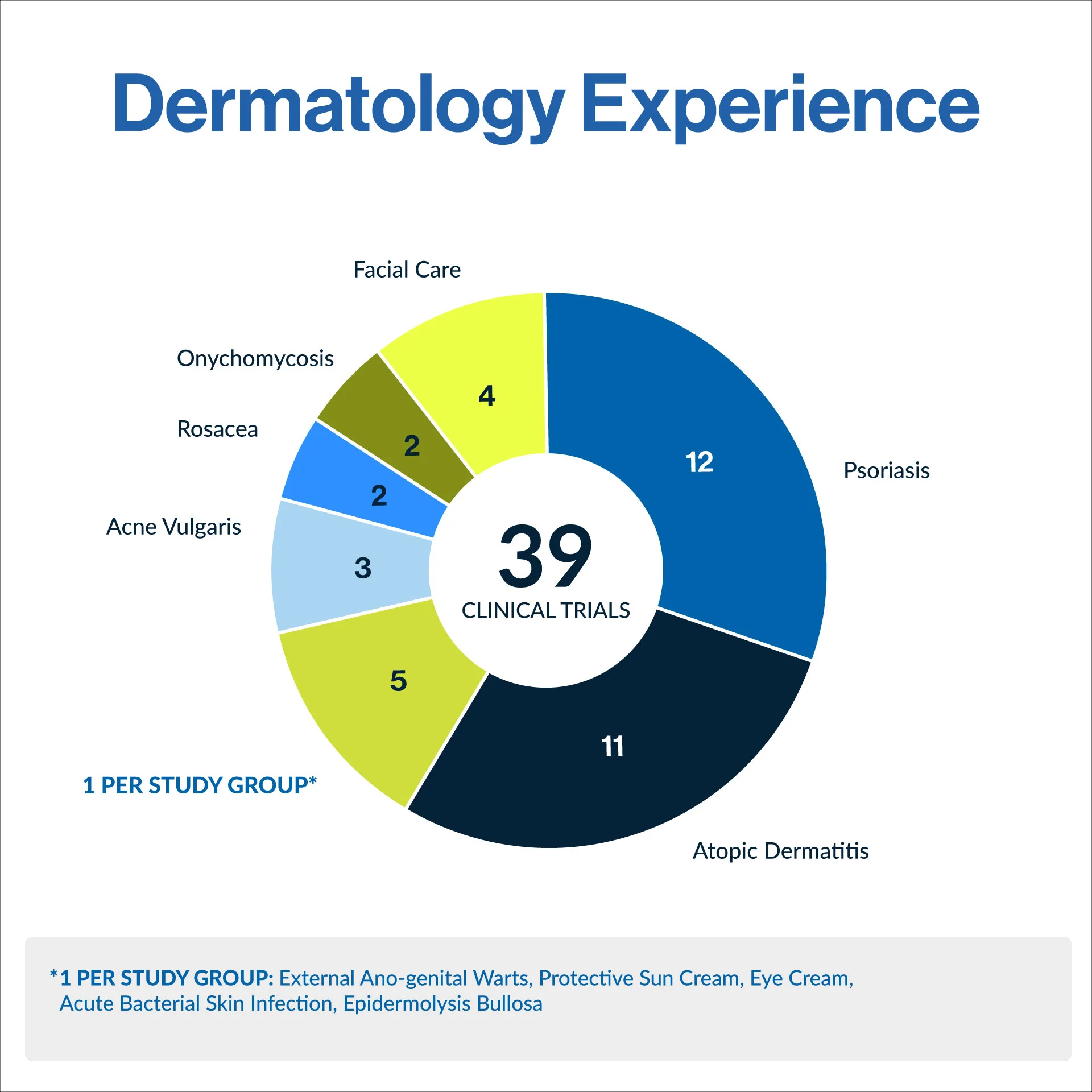
As demonstrated in the above chart, our experience ranges from atopic dermatitis and psoriasis to several niche, specialised dermatology trials, including epidermolysis bullosa, rosacea, and onychomycosis. This diverse portfolio highlights our wide range of clinical trial therapeutic area expertise within the field of dermatology.
Comac Medical’s Atopic Dermatitis Success Story
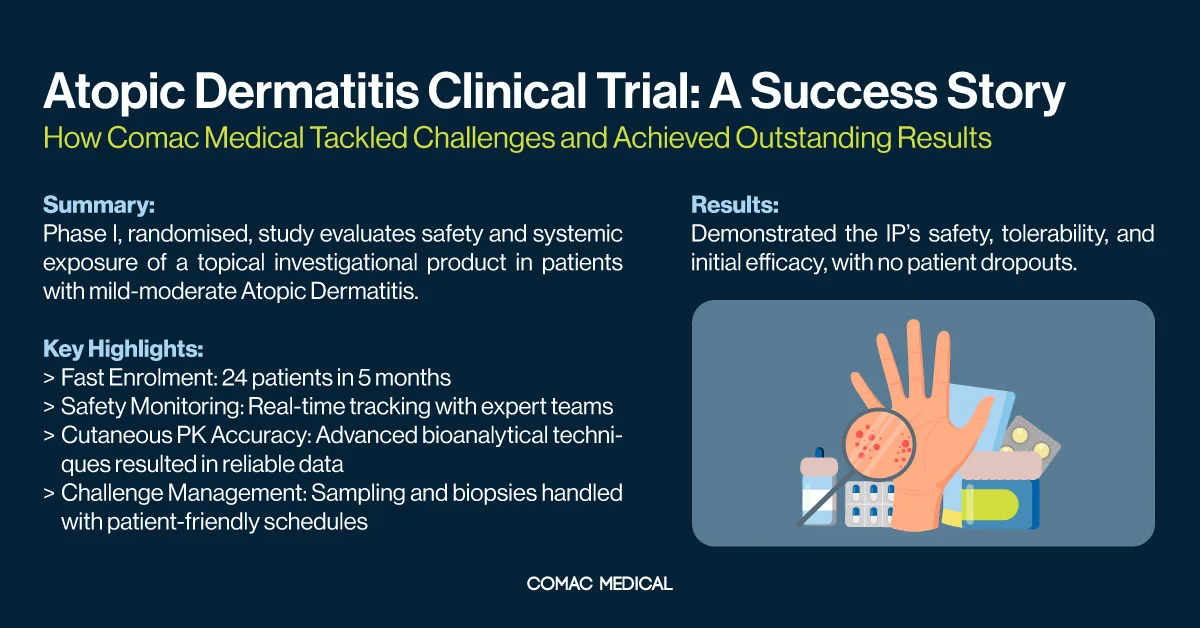
One of Comac Medical’s notable successes in dermatology clinical research is a Phase I clinical trial focused on atopic dermatitis. The study was designed as an investigator-blind, randomised, single-centre, vehicle-controlled, dose-escalation trial, conducted at our clinical research centre in Bulgaria. The trial involved 26 screened and 24 enrolled patients aged 18 to 60 with chronic mild to moderate atopic dermatitis. The treatment period lasted two weeks, and patient recruitment was completed within five months.
This early-phase trial presented several challenges, including intensive pharmacokinetic (PK) sampling, skin biopsies, and precise monitoring of systemic exposure. To overcome these obstacles, our team developed a tailored enrolment strategy and leveraged the expertise of experienced dermatologists and clinical pharmacologists. The successful collaboration ensured safe and accurate data collection while maintaining high patient retention.
This case study exemplifies our commitment to delivering high-quality dermatology clinical trials and highlights the critical role of collaboration between clinical experts and research professionals.
Advance Dermatology Treatment with Comac Medical
As dermatology clinical research evolves, Comac Medical remains committed to driving innovation in the field. In 2025, we are investing in expanding our current dermatology research to meet the growing demand for advanced treatments. Our team recently attended the American Academy of Dermatology (AAD) Conference in Orlando, where we explored new opportunities for collaboration and growth. With varied experience in dermatology trials, we are dedicated to overcoming the unique challenges in the field and improving patient outcomes.
We understand the unique challenges, from patient recruitment to high-quality data collection. Our network across Central and Eastern Europe offers access to diverse patient populations and streamlined regulatory processes, helping advance dermatology research and improve patient outcomes.
As chronic skin conditions rise, the need for high-quality clinical trials grows. Addressing these challenges requires collaboration among researchers, healthcare professionals, and CROs like Comac Medical. Through our efforts, we contribute to better patient care and the next generation of dermatology treatments.



